Finding Your Way Back to Yourself: Postpartum Depression Support in the Bay Area

You thought you had it all figured out. You're successful, driven, maybe you have that advanced degree hanging on your wall. You planned this pregnancy like you plan everything else in your life—with research, spreadsheets, and the best of intentions. But here you are, three months postpartum, staring at your beautiful baby and feeling... nothing. Or worse, feeling everything all at once—rage when they cry, guilt about not feeling joy, terror about being left alone with them.
At Bay Area Therapy for Wellness, we know this feeling: you're exhausted but can't sleep, even when the baby finally does. We understand you've bought every Montessori toy and researched the safest everything, yet still feel like you're failing. When your partner resumes their 'normal' life, we recognize you might be drowning in bottles and diapers, missing adult conversation but too overwhelmed for one more thing.
If this sounds familiar, you're not broken. You're experiencing postpartum depression, and you're certainly not alone among women in the Bay Area or anywhere else.
When "Baby Blues" Becomes Postpartum Depression
Everyone warned you about being tired. Everyone said the first few months would be hard. But nobody prepared you for this—feeling like a stranger in your own life, questioning whether you made a terrible mistake, or having scary thoughts that make you wonder if someone else should be raising your baby.
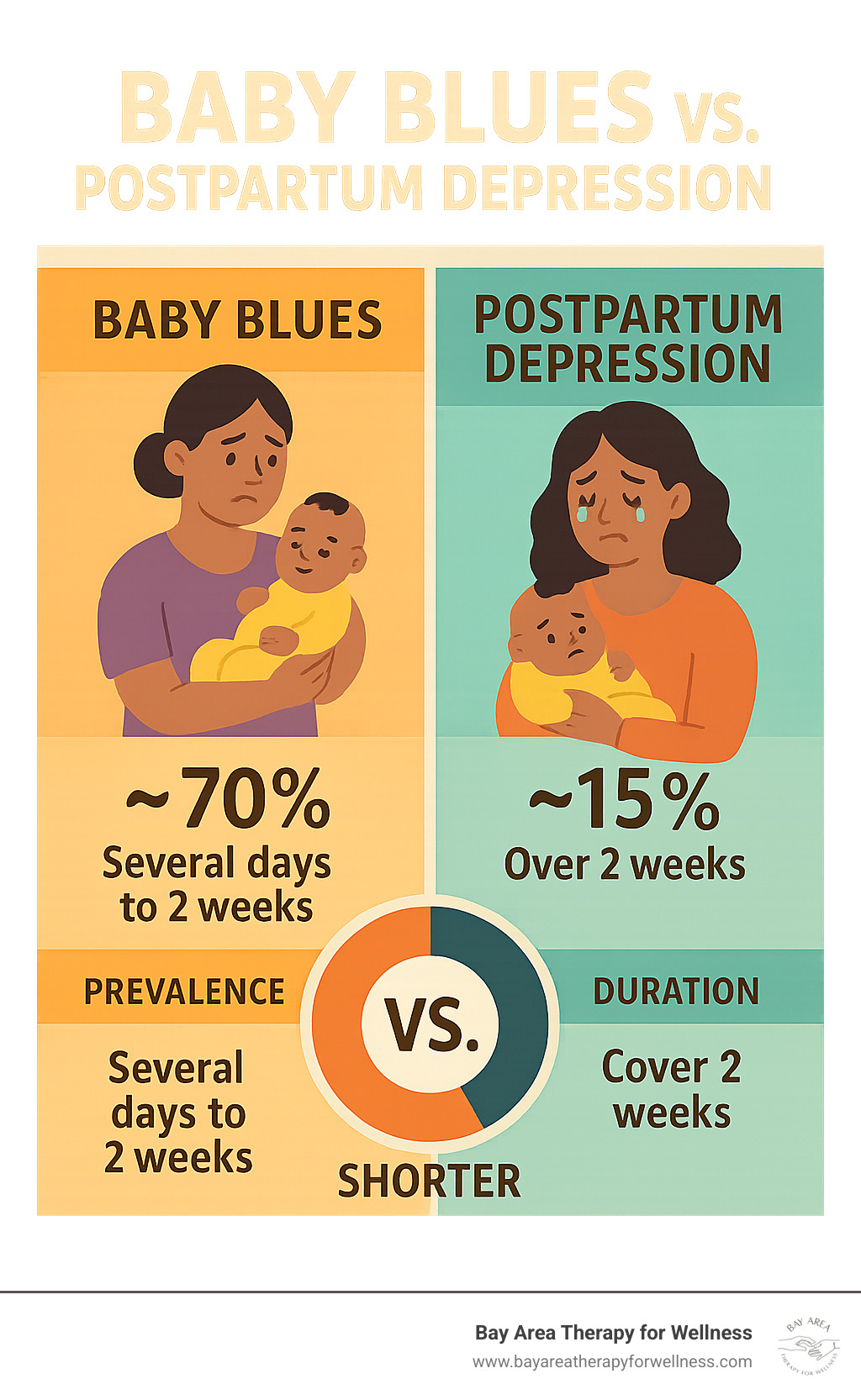
The baby blues affect up to 75% of new mothers and typically resolve within two weeks. You might cry more than usual, feel overwhelmed, or have mood swings during the postpartum period. This is your body adjusting to massive hormonal changes as estrogen and progesterone levels plummet after giving birth.
Postpartum depression is different from baby blues. It's more intense, lasts longer, and significantly impacts your ability to function. Postpartum depression can begin during pregnancy or up to a year after birth. Unlike baby blues that resolve on their own within two weeks, postpartum depression requires professional support and treatment to heal.
Postpartum depression often co-occurs with anxiety disorders, creating a complex web of symptoms that affect new mothers. Depression and anxiety during the postpartum period are common mental health conditions that many women experience, yet they often go unrecognized and untreated.
Here's what postpartum depression might look like for someone like you—a high-achieving woman in the Bay Area who's used to excelling at everything:
The Perfectionist's Struggle: You research everything obsessively because you want what's best for your baby, but nothing feels good enough. You're buying organic everything, following sleep schedules religiously, yet you feel like you're constantly failing at motherhood.
The Mental Challenge Void: You miss being intellectually stimulated. The repetitive nature of infant care feels suffocating when you're used to complex problem-solving and meaningful work.
The Identity Crisis: You don't recognize yourself. The confident, capable woman you were seems to have disappeared, replaced by someone who can't even decide what to have for lunch.
The Isolation Paradox: You want to get out and do things with your baby, but it feels impossible. You crave adult interaction but also feel too exhausted and overwhelmed to socialize with other parents.
The Sleep Trap: Even when your baby sleeps, you can't. You're hypervigilant, keeping one ear open, unable to truly rest because your nervous system won't let you.
Recognizing Postpartum Depression Symptoms in Your High-Achieving Life
Postpartum depression symptoms don't look the same for everyone, especially for women who are used to pushing through challenges and maintaining high standards. Understanding these symptoms is crucial for getting the postpartum depression support you need. You might be experiencing:
Persistent sadness or numbness that doesn't lift, even during good moments with your baby. You're going through the motions of care without feeling emotionally connected. This feeling sad experience extends beyond typical new parent emotions.
Overwhelming rage or irritability that surprises you with its intensity. You might snap at your partner or feel furious when the baby cries, then feel guilty about these reactions. This postpartum rage is a real symptom of postpartum depression.
Intrusive, scary thoughts about something happening to your baby—or worse, thoughts about harming yourself or your child. These symptoms are common with postpartum depression and anxiety disorders, not a reflection of who you are as a person.
Difficulty bonding with your baby, which creates additional guilt because you expected to feel that instant maternal connection everyone talks about. Many mothers struggle with bonding, and it doesn't mean you love your baby any less.
Changes in sleep and appetite beyond typical new parent exhaustion. You might be unable to sleep even when you have the opportunity, or you might be eating much more or less than usual. These physical symptoms often accompany postpartum depression.
Withdrawal from relationships because maintaining social connections feels too demanding when you're barely keeping your head above water. Many women with postpartum depression isolate themselves from friends and family members.
Guilt and worthlessness with a constant inner critic telling you that you're not cut out for this, that your baby deserves better, or that you should be handling this better than you are. These symptoms of depression and anxiety can be overwhelming.
If you're nodding along to these symptoms, especially if they've persisted for more than two weeks, seeking professional postpartum depression support is crucial. The longer postpartum depression goes untreated, the longer recovery can take.
Understanding Risk Factors and Perinatal Mood Disorders
Perinatal mood disorders, including postpartum depression and anxiety disorders, affect many women during pregnancy and the postpartum period. These are not rare experiences—postpartum depression is a common mental health condition that affects approximately one in seven new mothers.
Several risk factors can increase the likelihood of developing postpartum depression:
- Previous history of depression or anxiety disorders
- Family history of mental illness
- Lack of social support from family members and friends
- Stressful life events during pregnancy or after childbirth
- Complications during pregnancy or birth
- Hormonal changes after giving birth
- Sleep deprivation and physical exhaustion
Many women benefit from depression screening using tools like the Edinburgh Postnatal Depression Scale, which helps healthcare providers identify symptoms early and connect mothers with appropriate treatment options.

Why High-Achieving Bay Area Women Are Particularly Vulnerable
Living in the Bay Area comes with unique pressures that can exacerbate postpartum depression and anxiety. The culture of optimization and achievement that drives success in your career can become overwhelming when applied to motherhood.
You're surrounded by other high-achieving parents who seem to have it all figured out—the perfect nursery, the ideal feeding schedule, the seamless return to work. Social media feeds full of curated family moments can make your struggles with postpartum depression feel more isolating.
The cost of living in areas like San Francisco, Palo Alto, Menlo Park, and throughout the Peninsula adds financial stress. You might be weighing the costs of childcare against returning to work, or feeling pressure to maintain your career trajectory to afford your lifestyle. This stress can worsen symptoms of depression and anxiety.
The "having it all" mentality that's prevalent in Bay Area culture can make it harder to acknowledge when you need postpartum depression support. You're used to being the one who has answers, who solves problems, who excels at everything you do.
Professional Postpartum Depression Support That Gets It
When you're used to being competent and capable, admitting you need help can feel like the hardest thing you've ever done. But seeking professional support for postpartum depression isn't a sign of weakness—it's exactly what any smart, resourceful person would do when facing a mental health condition.
Virtual therapy throughout California means you can access specialized maternal mental health support from your home in Livermore, Pleasanton, Dublin, Danville, Walnut Creek, Lafayette, San Jose, Cupertino, Saratoga, Campbell, Los Gatos, Atherton, Redwood City, or anywhere else in the state. No commuting, no arranging childcare, no additional stress for new parents.
Treatment Options That Work for Postpartum Depression
Individual Therapy provides a safe space to process the complex emotions of postpartum depression without judgment. This isn't about someone sitting there nodding while you talk—it's an active, engaging process where you'll dig deep, process the hard stuff, and yes, even share some laughs along the way.
Cognitive Behavioral Therapy (CBT) helps challenge the negative thought patterns that fuel postpartum depression. When your inner critic is telling you you're a terrible mother, CBT provides tools to examine these thoughts objectively and develop more balanced perspectives.
Acceptance and Commitment Therapy (ACT) helps you accept difficult thoughts and feelings while committing to actions that align with your values. This treatment can be particularly powerful for high-achieving women who struggle with the loss of control that comes with new parenthood.
EMDR (Eye Movement Desensitization and Reprocessing) can be incredibly effective if you've experienced birth trauma, fertility struggles, or pregnancy loss. These experiences can compound postpartum depression, and EMDR helps process distressing memories to reduce their emotional impact.
Mindfulness-based approaches help you stay grounded in the present moment rather than spiraling into anxiety. These techniques are especially valuable for managing the hypervigilance that often accompanies postpartum depression and anxiety disorders.
The Role of Medication in Postpartum Depression Treatment
For some women, medication can provide crucial support in managing postpartum depression symptoms. Antidepressants can help stabilize mood and reduce anxiety, creating a foundation for therapy to be more effective in treating postpartum depression.
Many antidepressants are considered safe while breastfeeding, but this is always a conversation to have with your healthcare provider. The decision about medication is deeply personal and should be made based on your specific symptoms, circumstances, and preferences after a proper diagnosis.
Medication is often most effective when combined with talk therapy. It can help lift the heaviest symptoms of postpartum depression, allowing you to engage more fully in the therapeutic process and develop long-term coping skills.
Building Your Support Network: Resources for Mothers
You weren't meant to navigate new parenthood alone, even though it can feel isolating when you're struggling with postpartum depression. Building a strong support system is crucial for recovery from postpartum depression and preventing future episodes.
Partners and family members play a vital role in providing family support, but they need guidance on how to help effectively. It's not enough for someone to say "let me know if you need anything"—specific offers are more helpful. Instead of waiting for you to ask, other family members might say "I'm coming over Saturday morning to hold the baby while you shower and rest."
Support groups for mothers experiencing postpartum depression can provide validation and practical tips. These groups, whether in-person or virtual, connect you with other parents facing similar challenges with postpartum depression. Many women find that talking with other mothers who understand their struggles provides immense emotional support.
Professional childcare isn't a luxury—it's an investment in your mental health and well-being. Even a few hours a week can provide the breathing room you need to focus on recovery from postpartum depression.
Local resources and support groups in the Bay Area offer specialized help for mothers experiencing postpartum depression. These local support groups provide community connections and practical resources for families dealing with perinatal mood disorders.

Practical Strategies for Managing Postpartum Depression
While professional support is essential for treating postpartum depression, these strategies can help you manage symptoms in your daily life:
Prioritize self care and sleep above almost everything else. Ask your partner or family members to take night feedings so you can get longer stretches of rest. Sleep deprivation significantly worsens symptoms of postpartum depression and anxiety.
Nourish your body with regular, balanced meals. When you're struggling with postpartum depression, it's easy to skip meals or rely on quick fixes, but your brain needs proper nutrition to heal from depression and anxiety.
Move gently when you can. A short walk around your Livermore neighborhood or some gentle stretching can boost mood and energy without adding pressure to exercise intensely. Physical activity can help reduce symptoms of postpartum depression.
Practice grounding techniques when you feel overwhelmed by anxiety. Simple breathing exercises can help you stay present rather than spiraling into worry about everything you think you should be doing.
Lower your expectations temporarily. This isn't forever, but right now, "good enough" really is good enough. Your baby needs a healthy, healing mother more than they need everything to be perfect. Taking care of yourself is part of taking care of your child.
Create micro-moments of self care. Even 15 minutes alone for a hot shower or a cup of tea can help you reset and recharge when dealing with postpartum depression.
Understanding Resources Available for Postpartum Depression
Many women don't realize the extensive resources available for postpartum depression support. Understanding these resources can help you or someone you care about access the help needed for recovery.
Healthcare providers including obstetricians, pediatricians, and primary care doctors can provide depression screening and referrals to mental health specialists. Many healthcare providers now routinely screen for postpartum depression during postpartum visits.
Mental health professionals who specialize in perinatal mood disorders understand the unique challenges faced by new mothers. These specialists can provide targeted treatment for postpartum depression and anxiety disorders.
Support groups specifically for mothers with postpartum depression offer peer support and practical advice. Many groups meet both in-person and virtually, making them accessible to busy new parents.
Online resources provide immediate access to information about postpartum depression, treatment options, and coping strategies. These resources can be particularly helpful for women who may not be ready to seek in-person support.
Overcoming Barriers to Getting Postpartum Depression Support
Several factors might be keeping you from seeking the postpartum depression support you need:
Stigma and shame around mental health struggles can be particularly challenging for high-achieving women who are used to handling everything successfully. Remember that postpartum depression is a medical condition, not a personal failing.
The myth of maternal instinct suggests that loving and caring for your baby should come naturally. In reality, bonding is a process that can take time, especially when you're struggling with postpartum depression.
Fear of judgment from healthcare providers, family members, or other parents can keep you isolated. Working with a therapist who specializes in maternal mental health means you'll be understood, not judged for having postpartum depression.
Logistical challenges like arranging childcare or transportation are solved with virtual therapy. You can access postpartum depression support from your own home while your baby naps or plays nearby.
Concerns about breastfeeding and medication can be addressed with proper medical guidance. Many treatment options for postpartum depression are compatible with breastfeeding, and your healthcare providers can help you weigh the benefits and risks.

Supporting Partners and Families Affected by Postpartum Depression
Postpartum depression affects the whole family, not just the woman experiencing it directly. Partners often feel helpless, frustrated, or overwhelmed trying to support someone they love while managing their own stress and new parent responsibilities.
Communication is key when supporting someone with postpartum depression. Partners need to understand that postpartum depression is a medical condition, not something that can be fixed with logic or positive thinking. Listening without trying to solve everything can provide crucial emotional support.
Practical help matters more than words for families dealing with postpartum depression. Taking over night feedings, handling household tasks, or simply holding the baby while the struggling parent rests can provide tangible relief from the symptoms of postpartum depression.
Professional support for partners is also important when dealing with postpartum depression in the family. Watching someone you love struggle with depression and anxiety is emotionally draining, and partners need their own coping strategies and support systems.
Family therapy can help couples navigate this challenging period together, addressing communication patterns, expectations about parenting roles, and plans for moving forward as a family unit affected by postpartum depression.
Prevention and Early Intervention for Postpartum Depression
While not all cases of postpartum depression can be prevented, early intervention and awareness of risk factors can help reduce the severity and duration of symptoms. Understanding how to prevent postpartum depression or catch it early benefits both mothers and families.
Education about postpartum depression during pregnancy helps women and their families recognize symptoms early. Many pregnant women benefit from learning about the difference between baby blues and postpartum depression.
Building social support during pregnancy creates a foundation for the postpartum period. Having friends, family members, and healthcare providers who understand the signs of postpartum depression can lead to earlier treatment.
Depression screening during pregnancy and the postpartum period helps identify women at risk for postpartum depression. Regular screening allows healthcare providers to intervene early when symptoms of depression and anxiety first appear.
Stress management techniques learned during pregnancy can help women cope with the challenges of new parenthood and potentially reduce the risk of developing postpartum depression.
The Path Forward: What Recovery from Postpartum Depression Looks Like
Recovery from postpartum depression is absolutely possible. It's not about returning to exactly who you were before—you've been through a major life transition, and some change is natural and healthy. Instead, recovery means finding a new version of yourself that incorporates both your identity as a mother and your individual identity.
You'll start noticing small signs of improvement first when receiving treatment for postpartum depression. Maybe you find yourself genuinely laughing at something your partner says, or you feel a moment of real tenderness toward your baby. These moments will become more frequent as treatment for postpartum depression progresses.
Recovery means developing coping skills that will serve you throughout motherhood and beyond. You'll learn to recognize your triggers, manage stress more effectively, and ask for help when you need it. These skills are invaluable as you face future challenges in parenting and life, helping prevent postpartum depression in future pregnancies.
Most importantly, recovery from postpartum depression means reclaiming your sense of self while embracing this new role. You can be both a devoted mother and an individual with your own interests, goals, and identity. The two aren't mutually exclusive, and many women find they emerge stronger after treatment for postpartum depression.
Taking the First Step Toward Postpartum Depression Support
If you're ready to start your journey toward feeling like yourself again, the process begins with a consultation. This mandatory first step ensures that we're a good fit to work together and that I can provide the specialized postpartum depression support you need.
During our consultation, we'll discuss what's bringing you to therapy, and I'll assess whether I can help with your specific concerns related to postpartum depression. We'll also confirm that you're comfortable with virtual sessions and located in California, and address any questions about the process of treating postpartum depression.
If we decide to move forward, you'll be added to a secure client portal where you can complete all necessary paperwork electronically before our first session. If it's not the right fit, I'll provide referrals to other providers who might better meet your needs for postpartum depression support.
Sessions are engaging and collaborative when treating postpartum depression. You won't find a therapist who just sits there and nods—we'll dig deep into what you're experiencing, process difficult emotions, and work together to develop practical strategies for moving forward in your recovery from postpartum depression.
As a solo practitioner who specializes in maternal mental health, I understand the unique pressures faced by high-achieving women in the Bay Area struggling with postpartum depression. My approach is warm, non-judgmental, and tailored specifically to your needs and circumstances.
Virtual sessions mean you can access this specialized postpartum depression support from anywhere in California. Whether you're in San Francisco dealing with the pressures of city life, in Palo Alto navigating tech industry demands, or in Livermore trying to balance career and family while managing postpartum depression, help is available from your own home.
Your Journey to Wellness from Postpartum Depression Starts Now
You don't have to continue struggling with postpartum depression alone. Postpartum depression is treatable, and with the right support, you will feel like yourself again. The strength and determination that have served you well in other areas of your life will serve you in this recovery process from postpartum depression too.
Taking that first step to reach out for postpartum depression support isn't admitting defeat—it's exactly what any intelligent, resourceful person would do when facing a challenge that requires specialized expertise. You deserve to feel well, to enjoy your baby, and to experience the joy and fulfillment that can come with motherhood.
Your baby needs you to be healthy and healing from postpartum depression more than they need everything else to be perfect. By prioritizing your mental health and seeking treatment for postpartum depression, you're not only helping yourself—you're modeling self care and resilience for your child.
Recovery from postpartum depression is possible, hope is real, and support is available. Contact Bay Area Therapy for Wellness. Your journey back to yourself starts with recognizing that you deserve help and that asking for postpartum depression support is a sign of strength, not weakness.
